[ad_1]
Guan, W. et al. Clinical characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 382, 1708–1720 (2020).
Goyal, P. et al. Clinical characteristics of Covid-19 in New York City. N. Engl. J. Med. 382, 2372–2374 (2020).
Giacomelli, A. et al. Self-reported olfactory and taste disorders in patients with Severe Acute Respiratory Coronavirus 2 Infection: A cross-sectional study. Clin. Infect. Dis. 71, 889–890 (2020).
Spinato, G. et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA 323, 2089–2090 (2020).
Lechien, J. R. et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur. Arch. Otorhinolaryngol. 277, 2251–2261 (2020).
Menni, C. et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat. Med. 26, 1037–1040 (2020).
Kaye, R., Chang, C. W. D., Kazahaya, K., Brereton, J. & Denneny, J. C. COVID-19 anosmia reporting tool: Initial findings. Otolaryngol. Neck Surg. 163, 132–134 (2020).
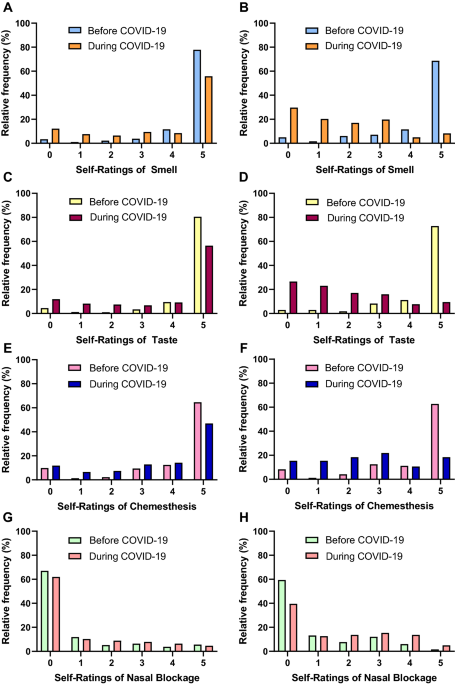
Parma, V. et al. More than smell—COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chem. Senses 45, 609–622 (2020).
Mao, L. et al. Neurologic manifestations of hospitalized patients with Coronavirus Disease 2019 in Wuhan China. JAMA Neurol. 77, 683–690 (2020).
Lee, Y., Min, P., Lee, S. & Kim, S. W. Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J. Korean Med. Sci. 35, e174 (2020).
Tham, A. C. et al. Olfactory taste disorder as a presenting symptom of COVID-19: A large single-center Singapore study. Eur. Arch. Otorhinolaryngol. 278, 1853–1862 (2021).
Butowt, R., Bilinska, K. & Von Bartheld, C. S. Chemosensory dysfunction in COVID-19: Integration of genetic and epidemiological data points to D614G spike protein variant as a contributing factor. ACS Chem. Neurosci. 11, 3180–3184 (2020).
Von Bartheld, C. S., Butowt, R. & Hagen, M. M. Prevalence of chemosensory dysfunction in COVID-19 patients: A systematic review and meta-analysis reveals significant ethnic differences. ACS Chem. Neurosci. 11, 2944–2961 (2020).
Lemeshow, S., Hosmer, D. W., Klar, J. & Lwanga, S. K. Adequacy of sample size in health studies. (John Wiley & Sons, Inc., 1990).
Lê, S., Josse, J. & Husson, F. FactoMineR: An R package for multivariate analysis. J. Stat. Softw. 25, 1–18 (2008).
Sim, B. L. H. et al. Clinical characteristics and risk factors for severe COVID-19 infections in Malaysia: A nationwide observational study. Lancet Reg. Heal. West. Pacific 4, 100055 (2020).
Ng, B. H. et al. COVID-19 detected from targeted contact tracing, attempting to see the pattern in random happenings: Early lessons in Malaysia. Med. J. Malaysia 75, 582–584 (2020).
Ramasamy, K., Saniasiaya, J. & Abdul Gani, N. Olfactory and gustatory dysfunctions as a clinical manifestation of Coronavirus Disease 2019 in a Malaysian tertiary center. Ann. Otol. Rhinol. Laryngol. 130, 513–519 (2021).
Violán, C. et al. Comparison of the information provided by electronic health records data and a population health survey to estimate prevalence of selected health conditions and multimorbidity. BMC Public Health 13, 251 (2013).
Basch, E. et al. Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: Results of a questionnaire-based study. Lancet Oncol. 7, 903–909 (2006).
Fromme, E. K., Eilers, K. M., Mori, M., Hsieh, Y. C. & Beer, T. M. How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the Quality-of-Life Questionnaire C30. J. Clin. Oncol. 22, 3485–3490 (2004).
Hopkins, C. et al. Six month follow-up of self-reported loss of smell during the COVID-19 pandemic. Rhinology 59, 26–31 (2021).
Majid, A., Burenhult, N., Stensmyr, M., De Valk, J. & Hansson, B. S. Olfactory language and abstraction across cultures. Philos. Trans. R. Soc. B Biol. Sci. 373, 20170139 (2018).
Majid, A. Human olfaction at the intersection of language, culture, and biology. Trends Cogn. Sci. 25, 111–123 (2021).
Baharuddin, A. R. & Sharifudin. The impact of geographical location on taste sensitivity and preference. Int. Food Res. J. 22, 731–738 (2015).
Von Bartheld, C. S., Hagen, M. M. & Butowt, R. The D614G virus mutation enhances anosmia in COVID-19 patients: Evidence from a systematic review and meta-analysis of studies from South Asia. ACS Chem. Neurosci. 12, 3535–3549 (2021).
Soh, S. H. L. et al. Prevalence of olfactory and taste dysfunction in COVID-19 patients: A community care facility study. Eur. Arch. Otorhinolaryngol. 278, 3375–3380 (2021).
See, A., Ko, K. K. K. & Toh, S. T. Epidemiological analysis in support of hypothesis that D614G virus mutation is a major contributing factor to chemosensory dysfunction in COVID-19 patients. Eur. Arch. Otorhinolaryngol. 278, 3595–3596 (2021).
Chong, Y. M. et al. SARS-CoV-2 lineage B.6 was the major contributor to early pandemic transmission in Malaysia. PLoS Negl. Trop. Dis. 14, 1–12 (2020).
Mat Yassim, A. S. et al. COVID-19 outbreak in Malaysia: Decoding D614G mutation of SARS-CoV-2 virus isolated from an asymptomatic case in Pahang. Mater. Today Proc. https://doi.org/10.1016/j.matpr.2021.02.387 (2021).
Sudre, C. et al. Symptom clusters in COVID-19: a potential clinical prediction tool from the COVID Symptom study app. Preprint at medRxiv https://doi.org/10.1101/2020.06.12.20129056 (2020).
Elliott, J. et al. Symptom reporting in over 1 million people: community detection of COVID-19. Preprint at medRxiv https://doi.org/10.1101/2021.02.10.21251480 (2021).
Sungnak, W. et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat. Med. 26, 681–687 (2020).
Xiao, F. et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology 158, 1831-1833.e3 (2020).
Eliezer, M. et al. Sudden and complete olfactory loss of function as a possible symptom of COVID-19. JAMA Otolaryngol. Neck Surg. 146, 674–675 (2020).
Bilinska, K., Jakubowska, P., Von Bartheld, C. S. & Butowt, R. Expression of the SARS-CoV-2 entry proteins, ACE2 and TMPRSS2, in cells of the olfactory epithelium: Identification of cell types and trends with age. ACS Chem. Neurosci. 11, 1555–1562 (2020).
Brann, D. H. et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Sci. Adv. 6, 5801–5832 (2020).
Zheng, J. et al. COVID-19 treatments and pathogenesis including anosmia in K18-hACE2 mice. Nature 589, 603–607 (2021).
Cazzolla, A. P. et al. Taste and smell disorders in COVID-19 patients: Role of interleukin-6. ACS Chem. Neurosci. 11, 2774–2781 (2020).
Rodriguez, S. et al. Innate immune signaling in the olfactory epithelium reduces odorant receptor levels: Modeling transient smell loss in COVID-19 patients. Preprint at medRxiv https://doi.org/10.1101/2020.06.14.20131128 (2020).
Butowt, R., Meunier, N., Bryche, B. & von Bartheld, C. S. The olfactory nerve is not a likely route to brain infection in COVID-19: A critical review of data from humans and animal models. Acta Neuropathol. 141, 809–822 (2021).
Sato, T. et al. Expression of ACE2 and TMPRSS2 proteins in the upper and lower aerodigestive tracts of rats: Implications on COVID 19 Infections. Laryngoscope 131, E932–E939 (2021).
Xu, H. et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral Sci. 12, 8 (2020).
Lechien, J. R. et al. Loss of smell and taste in 2013 european patients with mild to moderate covid-19. Ann. Intern. Med. 173, 672–675 (2020).
Vaira, L. A. et al. Olfactory and gustatory function impairment in COVID-19 patients: Italian objective multicenter-study. Head Neck 42, 1560–1569 (2020).
Moein, S. T. et al. Smell dysfunction: A biomarker for COVID-19. Int. Forum Allergy Rhinol. 10, 944–950 (2020).
Hintschich, C. A. et al. Psychophysical tests reveal impaired olfaction but preserved gustation in COVID-19 patients. Int. Forum Allergy Rhinol. 10, 1105–1107 (2020).
Lötsch, J. & Hummel, T. Clinical usefulness of self-rated olfactory performance—a data science-based assessment of 6000 patients. Chem. Senses 44, 357–364 (2019).
Hoffman, H. J., Rawal, S., Li, C. M. & Duffy, V. B. New chemosensory component in the US National Health and Nutrition Examination Survey (NHANES): first-year results for measured olfactory dysfunction. Rev. Endocr. Metab. Disord. 17, 221–240 (2016).
Boscutti, A. et al. Olfactory and gustatory dysfunctions in SARS-CoV-2 infection: a systematic review. Brain, Behav. Immun. – Heal. 15, 100268 (2021).
Gerkin, R. C. et al. Recent smell loss is the best predictor of COVID-19 among individuals with recent respiratory symptoms. Chem. Senses 46, bjaa081 (2021).
Cecchetto, C. et al. Assessing the extent and timing of chemosensory impairments during COVID-19 pandemic. Sci. Rep. 11, 17504 (2021).
Sai-Guan, L., Husain, S., Zahedi, F. D., Ahmad, N. & Gendeh, B. S. Cultural adaptation of Sniffin’ Sticks smell identification test: the Malaysian version. Iran. J. Otorhinolaryngol. 32, 213–222 (2020).
阅读更多